| Home | Sources Directory | News Releases | Calendar | Articles | | Contact | |
Assisted reproductive technology
Assisted reproductive technology (ART) is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons. ART is also used in couples who are discordant for certain communicable diseases, i.e. AIDS, to reduce the risk of infection when a pregnancy is desired. The term includes any reproductive technique involving a third party e.g. a sperm donor. There is yet no strict definition of the term. Usage of the ART mainly belongs in the field of reproductive endocrinology and infertility.
Contents |
[edit] Definitions
While there is no consensus on the definition, generally the process of intercourse is bypassed either by insemination (for example, artificial insemination) or fertilization of the oocytes in the laboratory environment (i.e. in vitro fertilisation).
- The Centers for Disease Control and Prevention (CDC)'which is required as a result of the 1992 Fertility Clinic Success Rate and Certification Act to publish the annual ART success rates at U.S. fertility clinics'defines ART to include "all fertility treatments in which both eggs and sperm are handled. In general, ART procedures involve surgically removing eggs from a woman's ovaries, combining them with sperm in the laboratory, and returning them to the woman's body or donating them to another woman." According to CDC, "they do not include treatments in which only sperm are handled (i.e., intrauterine'or artificial'insemination) or procedures in which a woman takes medicine only to stimulate egg production without the intention of having eggs retrieved."
[edit] Procedures
Procedures are mainly fertility medication, as well as ART techniques that use more substantial and forceful interventions, of which in vitro fertilization (IVF) and expansions of it (e.g. OCR, AZH, ICSI, ZIFT) are the most prevalent. However, there are also other manual ART, not necessarily dependent on IVF (e.g. PGD, GIFT, SSR).
[edit] Medication
Most fertility medication are agents that stimulate the development of follicles in the ovary. Examples are gonadotropins and gonadotropin releasing hormone.
[edit] In vitro fertilization
In vitro fertilization (IVF) is the technique of letting fertilization of the male and female gametes (sperm and egg) occur outside the female body.
Embryo transfer is the step in the process whereby one or several embryos are placed into the uterus of the female with the intent to establish a pregnancy.
[edit] Expansions of IVF
The following are techniques involved in, or requiring, in vitro fertilisation. In vitro fertilization does not necessarily involve each technique.
- Transvaginal ovum retrieval (OCR) is the process whereby a small needle is inserted through the back of the vagina and guided via ultrasound into the ovarian follicles to collect the fluid that contains the eggs.
- Assisted zona hatching (AZH) is performed shortly before the embryo is transferred to the uterus. A small opening is made in the outer layer surrounding the egg in order to help the embryo hatch out and aid in the implantation process of the growing embryo.
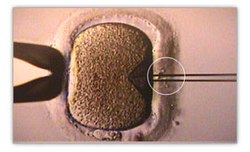
- Intracytoplasmic sperm injection (ICSI) is beneficial in the case of male factor infertility where sperm counts are very low or failed fertilization occurred with previous IVF attempt(s). The ICSI procedure involves a single sperm carefully injected into the center of an egg using a microneedle. This method is also sometimes employed when donor sperm is used.
- Autologous endometrial coculture is a possible treatment for patients who have failed previous IVF attempts or who have poor embryo quality. The patient's fertilized eggs are placed on top of a layer of cells from the patient's own uterine lining, creating a more natural environment for embryo development.
- In zygote intrafallopian transfer (ZIFT), egg cells are removed from the woman's ovaries and fertilized in the laboratory; the resulting zygote is then placed into the fallopian tube.
- Cytoplasmic transfer is the technique in which the contents of a fertile egg from a donor are injected into the infertile egg of the patient along with the sperm.
- Egg donors are resources for women with no eggs due to surgery, chemotherapy, or genetic causes; or with poor egg quality, previously unsuccessful IVF cycles or advanced maternal age. In the egg donor process, eggs are retrieved from a donor's ovaries, fertilized in the laboratory with the sperm from the recipient's partner, and the resulting healthy embryos are returned to the recipient's uterus.
- A gestational carrier is an option when a patient's medical condition prevents a safe pregnancy, when a patient has ovaries but no uterus due to congenital absence or previous surgical removal, and where a patient has no ovaries and is also unable to carry a pregnancy to full term.
- Preimplantation genetic diagnosis (PGD) involves the use of genetic screening mechanisms such as Fluorescent In Situ Hybridization (FISH) or Comparative Genomic Hybridization (CGH) to help identify genetically abnormal embryos and improve healthy outcomes.
- Embryo splitting can be used for twinning to increase the number of available embryos.[1]
[edit] Others
The following Assisted Reproduction techniques don't necessarily involve IVF.
- In gamete intrafallopian transfer (GIFT) a mixture of sperm and eggs is placed directly into a woman's fallopian tubes using laparoscopy following a transvaginal ovum retrieval.
- Sex selection is the attempt to control the sex of offspring to achieve a desired sex. It can be accomplished in several ways, both pre- and post-implantation of an embryo, as well as at birth. Pre-implantation techniques include PGD, but also sperm sorting.
- Artificial insemination (AI) is when sperm is placed into a female's uterus (intrauterine) or cervix (intracervical) using artificial means rather than by natural copulation.
- Conception devices, such as a conception cap are used to aid conception by enhancing[vague] the natural process. Conception caps are used by placing semen into a small conception cap, then placing the cap onto the cervix. This holds the semen at the cervical os, protecting the semen from the acidic vaginal secretions and keeping it in contact with the cervical mucus.
- Artificial insemination by donor is used in situations where the woman doesn't have a partner with functional sperm. Instead, a sperm donor supplies the sperm.
- Surrogacy, where a woman agrees to become pregnant and deliver a child for a contracted party. It may be her own biological child, or a child conceived through in vitro fertilization or embryo transfer using another woman's ova.
- Reproductive surgery, treating e.g. fallopian tube obstruction and vas deferens obstruction, or reversing a vasectomy by a reverse vasectomy.
- In surgical sperm retrieval (SSR) the reproductive urologist obtains sperm from the vas deferens, epididymis or directly from the testis in a short outpatient procedure.
- By cryopreservation, eggs, sperm and reproductive tissue can be preserved for later IVF.
[edit] Risks
The majority of IVF-conceived infants do not have birth defects.[2] However, some studies have suggested that assisted reproductive technology is associated with an increased risk of birth defects.[3][4] In the largest U.S. study, which used data from a statewide registry of birth defects,[5] 6.2% of IVF-conceived children had major defects, as compared with 4.4% of naturally conceived children matched for maternal age and other factors (odds ratio, 1.3; 95% confidence interval, 1.00 to 1.67).[2]
The main risks are:
- Genetic disorders. DNA damage increases in e.g. IVF and ICSI, which is reflected e.g. by upregulation of the gene expression of HNRNPC in the placenta.[6]
- Low birth weight. In IVF and ICSI, a risk factor is the decreased expression of proteins in energy metabolism; Ferritin light chain and ATP5A1.[6]
- Preterm birth. Low birth weight and preterm birth are strongly associated with many health problems, such as visual impairment and cerebral palsy, and children born after IVF are roughly twice as likely to have cerebral palsy.[7]
Other risk factors are:
- Membrane damage, which is contributed to or reflected by increased expression of the membrane fusion proteins NAPA and Annexin A3[6].
Sperm donation is an exception, with a birth defect rate of almost a fifth compared to the general population.[8] It may be explained by that sperm banks accept only people with high sperm count.
[edit] Usage
Assisted reproductive technology procedures performed in the U.S. has more than doubled since 10 years ago, with 140.000 procedures in 2006[9], resulting in 55.000 infants born.[9]
In Australia, 3.1 percent of babies now born are a result of ART.[10]
[edit] Costs
[edit] United States of America
Not everyone in the U.S. has insurance coverage for fertility investigations and treatments. Many states are starting to mandate coverage, and the rate of utilization is 277% higher in states with complete coverage.[11]
There are some health insurance companies that cover diagnosis of infertility but frequently once diagnosed will not cover any treatment costs.
2005 approximate treatment/diagnosis costs (United States, costs in US$):
- Initial workup: hysteroscopy, hysterosalpingogram, blood tests ~$2,000
- Intrauterine Insemination (IUI) fka Artificial insemination ~ $200' 900 per. trial
- Sonohysterogram (SHG) ~ $600 ' 1,000
- Clomiphene citrate cycle ~ $ 200 - 500
- IVF cycle ~ $10,000 -30,000
- Use of a surrogate mother to carry the child - dependent on arrangements
Another way to look at costs is to determine the cost of establishing a pregnancy. Thus if a clomiphene treatment has a chance to establish a pregnancy in 8% of cycles and costs $500, it will cost ~ $6,000 to establish a pregnancy, compared to an IVF cycle (cycle fecundity 40%) with a corresponding cost of ($12,000/40%) $30,000
For the community as a whole, the cost of IVF on average pays back by 700% by tax from future employment by the conceived human being.[12]
[edit] United Kingdom
In the UK all patients have the right to preliminary testing, provided free of charge by the National Health Service. However, treatment is not widely available on the NHS and there can be long waiting lists. Many patients therefore pay for immediate treatment within the NHS or seek help from private clinics[13].
[edit] Sweden
In Sweden, official fertility clinics provide most necessary treatments and initial workup, but there are long waiting lists, especially for egg donations, since the donor gets just as low reward as the receiving couple are charged. However, there are private fertility clinics.[citation needed]
[edit] Canada
Some treatments are covered by OHIP (public health insurance) in Ontario and others are not. If you are undergoing artificial insemination or if you have bilaterally blocked fallopian tubes and are under 40, the treatment is covered but you are still required to pay lab fees which are around $3,000-4,000. Coverage would vary in other provinces. Most other patients are required to pay for treatments themselves.[14]
[edit] Israel
Israel's National Health Insurance, which is mandatory for all Israeli citizens, covers nearly all fertility treatments. In-Vitro-Fertilization costs are fully subsidized up to the birth of two children for all Israeli women, including single women and lesbian couples. Embryo transfers for purposes of gestational surrogacy are also covered.[15]
[edit] New Zealand
The national public health system of New Zealand covers IVF treatment in specific circumstances only, based on a 'points for conception challenges' equation.[citation needed] Publicly funded IVF treatments are limited (between one and three treatments dependent on criteria) and are subject to substantial wait-lists, dependent on local health funding region, which raises potential inequity of ART support across the country.[citation needed] Infertility testing through blood tests can be covered by public funding, however in the absence of explicit gynecological complications, additional investigations are may not be covered publicly. Investigation such as a hysterosalpingogram may be covered, but the wait-list could be in excess of six weeks, whereas a privately sourced HSG can cost $NZ900 but is readily available. Many New Zealanders select self-funded IVF cycles, at approximately $NZ10,000 per cycle, and other forms of ART, such as IUI, at approximately $NZ1200, using the services of private fertility clinics, which in itself is a growing local industry. Individuals using private services are generally not covered under personal health insurance policies in New Zealand.
[edit] Ethics
Some couples find it difficult to stop treatment despite very bad prognosis, resulting in futile therapies. This may give ART providers a difficult decision of whether to continue or refuse treatment.[16]
For treatment-specific ethical considerations, see entries in individual subarticles, e.g. In vitro fertilisation, Surrogacy and Sperm donation
[edit] Fictional representation
Films and other fiction depicting emotional struggles of assisted reproductive technology have had an upswing in the latter part of the 2000s decade, although the techniques have been available for decades.[17] Yet, the amount of people that can relate to it by personal experience in one way or another is ever growing, and the variety of trials and struggles are huge.[17]
For specific examples, refer to the fiction sections in individual subarticles, e.g. surrogacy, sperm donation and fertility clinic.
In addition, reproduction and pregnancy in speculative fiction has been present for many decades.
[edit] See also
[edit] References
- ^ Illmensee K, Levanduski M, Vidali A, Husami N, Goudas VT (February 2009). "Human embryo twinning with applications in reproductive medicine". Fertil. Steril. 93 (2): 423'7. doi:10.1016/j.fertnstert.2008.12.098. PMID 19217091.
- ^ a b Van Voorhis BJ (2007). "Clinical practice. In vitro fertilization". N Engl J Med 356 (4): 379'86. doi:10.1056/NEJMcp065743. PMID 17251534.
- ^ Kurinczuk JJ, Hansen M, Bower C (2004). "The risk of birth defects in children born after assisted reproductive technologies". Curr Opin Obstet Gynecol 16 (3): 201'9. doi:10.1097/00001703-200406000-00002. PMID 15129049.
- ^ Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ (2005). "Assisted reproductive technologies and the risk of birth defects--a systematic review". Hum Reprod 20 (2): 328'38. doi:10.1093/humrep/deh593. PMID 15567881. http://humrep.oxfordjournals.org/cgi/reprint/20/2/328.pdf.
- ^ Olson CK, Keppler-Noreuil KM, Romitti PA, Budelier WT, Ryan G, Sparks AE, Van Voorhis BJ (2005). "In vitro fertilization is associated with an increase in major birth defects". Fertil Steril 84 (5): 1308'15. doi:10.1016/j.fertnstert.2005.03.086. PMID 16275219.
- ^ a b c Zhang Y, Zhang YL, Feng C, et al. (September 2008). "Comparative proteomic analysis of human placenta derived from assisted reproductive technology". Proteomics 8 (20): 4344. doi:10.1002/pmic.200800294. PMID 18792929.
- ^ Hvidtjørn D, Schieve L, Schendel D, Jacobsson B, Sværke C, Thorsen P (2009). "Cerebral palsy, autism spectrum disorders, and developmental delay in children born after assisted conception: a systematic review and meta-analysis". Arch Pediatr Adolesc Med 163 (1): 72'83. doi:10.1001/archpediatrics.2008.507. PMID 19124707. http://archpedi.ama-assn.org/cgi/content/full/163/1/72.
- ^ motherearthnews.com - THE SPERM CRISIS
- ^ a b chicagotribune.com Infertility by the numbers Colleen Mastony. June 21, 2009
- ^ 'More IVF babies but less multiple births' THE AUSTRALIAN. September 24, 2009
- ^ Jain T, Harlow BL, Hornstein MD. "Insurance coverage and outcome of in vitro fertilization." New England Journal of Medicine. 347(9):661-6.
- ^ Long-term Economic Benefits Attributed to IVF-conceived Children: A Lifetime Tax Calculation by Mark P. Connolly, MHE; Michael S. Pollard, PhD; Stijn Hoorens, MSc; Brian R. Kaplan, MD; Selwyn P. Oskowitz, MD; and Sherman J. Silber, MD
- ^ Infertility Treatment, NHS Direct Online (NHS Direct Online Health Enyclopaedia)
- ^ IVF Canada
- ^ Teman, Elly. 2010. Birthing a Mother: the Surrogate Body and the Pregnant Self. Berkeley: University of California Press
- ^ Fertility treatment when the prognosis is very poor or futile. Fertil Steril. 2009 Aug 31. PMID: 19726040
- ^ a b chicagotribune.com --> Heartache of infertility shared on stage, screen By Colleen Mastony, Tribune reporter. June 21, 2009
[edit] External links
- Centers for Disease Control and Prevention (CDC), Assisted Reproductive Technology
- The ethical aspects of gamete micromanipulation
- American Society for Reproductive Medicine
- Society for Assisted Reproductive Technology
|
||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||
|
SOURCES.COM is an online portal and directory for journalists, news media, researchers and anyone seeking experts, spokespersons, and reliable information resources. Use SOURCES.COM to find experts, media contacts, news releases, background information, scientists, officials, speakers, newsmakers, spokespeople, talk show guests, story ideas, research studies, databases, universities, associations and NGOs, businesses, government spokespeople. Indexing and search applications by Ulli Diemer and Chris DeFreitas.
For information about being included in SOURCES as a expert or spokesperson see the FAQ . For partnerships, content and applications, and domain name opportunities contact us.