| Home | Sources Directory | News Releases | Calendar | Articles | | Contact | |
Interferon
Interferons (IFNs) are proteins made and released by lymphocytes in response to the presence of pathogens'such as viruses, bacteria, or parasites'or tumor cells. They allow communication between cells to trigger the protective defenses of the immune system that eradicate pathogens or tumors.
IFNs belong to the large class of glycoproteins known as cytokines. Interferons are named after their ability to "interfere" with viral replication within host cells. IFNs have other functions: they activate immune cells, such as natural killer cells and macrophages; they increase recognition of infection or tumor cells by up-regulating antigen presentation to T lymphocytes; and they increase the ability of uninfected host cells to resist new infection by virus. Certain host symptoms, such as aching muscles and fever, are related to the production of IFNs during infection.
About ten distinct IFNs have been identified in mammals; seven of these have been described for humans. They are typically divided among three IFN classes: Type I IFN, Type II IFN, and Type III IFN. IFNs belonging to all IFN classes are very important for fighting viral infections.
Contents |
[edit] Types of interferon
Based on the type of receptor through which they signal, human interferons have been classified into three major types.
- Interferon type I: All type I IFNs bind to a specific cell surface receptor complex known as the IFN-î� receptor (IFNAR) that consists of IFNAR1 and IFNAR2 chains. The type I interferons present in humans are IFN-î�, IFN-î� and IFN-ω.[1]
- Interferon type II: Binds to IFNGR. In humans this is IFN-î�.
- Interferon type III: Signal through a receptor complex consisting of IL10R2 (also called CRF2-4) and IFNLR1 (also called CRF2-12). Acceptance of this classification is less universal than that of type I and type II, and unlike the other two, it is not currently included in Medical Subject Headings.[2]
[edit] Function
All interferons share several common effects; they are antiviral agents and can fight tumors.
As an infected cell dies from a cytolytic virus, viral particles are released that can infect nearby cells. However, the infected cell can warn neighboring cells of a viral presence by releasing interferon. The neighboring cells, in response to interferon, produce large amounts of an enzyme known as protein kinase R (PKR). This enzyme phosphorylates a protein known as eIF-2 in response to new viral infections; eIF-2 is a eukaryotic translation initiation factor that forms an inactive complex with another protein, called eIF2B, to reduce protein synthesis within the cell. Another cellular enzyme, RNAse L'also induced following PKR activation'destroys RNA within the cells to further reduce protein synthesis of both viral and host genes. Inhibited protein synthesis destroys both the virus and infected host cells. In addition, interferons induce production of hundreds of other proteins ' known collectively as interferon-stimulated genes (ISGs)'that have roles in combating viruses.[3][4] They also limit viral spread by increasing p53 activity, which kills virus-infected cells by promoting apoptosis.[5][6] The effect of IFN on p53 is also linked to its protective role against certain cancers.[5]
Another function of interferon is to upregulate major histocompatibility complex molecules, MHC I and MHC II, and increase immunoproteasome activity. Higher MHC I expression increases presentation of viral peptides to cytotoxic T cells, while the immunoproteasome processes viral peptides for loading onto the MHC I molecule, thereby increasing the recognition and killing of infected cells by T cells. Higher MHC II expression increases presentation of viral peptides to helper T cells; these cells release cytokines that signal to and co-ordinate the activity of other cells of the immune system. Interferons directly activate some other immune cells, such as macrophages and natural killer cells.
[edit] Induction of interferons
Production of interferons predominantly occurs in response to microbes, such as viruses and bacteria, and their products. Binding of molecules uniquely found in microbes'viral glycoproteins, viral RNA, bacterial endotoxin (lipopolysaccharide), bacterial flagella, CpG motifs--by pattern recognition receptors, such as membrane bound Toll like receptors or the cytoplasmic receptors RIG-I or MDA5, can trigger release of IFNs. Toll Like Receptor 3 (TLR3) is important for inducing interferon in response to the presence of double-stranded RNA viruses; the ligand for this receptor is double-stranded RNA (dsRNA). After binding dsRNA, this receptor activates the transcription factors IRF3 and NF-î�B, which are important for initiating synthesis of many inflammatory proteins. Release of IFN from cells is also induced by mitogens. Other cytokines, such as interleukin 1, interleukin 2, interleukin-12, tumor necrosis factor and colony-stimulating factor, can also enhance interferon production.[7]
[edit] Downstream signaling
By interacting with their specific receptors, IFNs activate signal transducer and activator of transcription (STAT) complexes; STATs are a family of transcription factors that regulate the expression of certain immune system genes. Some STATs are activated by both type I and type II IFNs. However each IFN type can also activate unique STATs.[8]
STAT activation initiates the most well-defined cell signaling pathway for all IFNs, the classical Janus kinase-STAT (JAK-STAT) signaling pathway.[8] In this pathway, JAKs associate with IFN receptors and, following receptor engagement with IFN, phosphorylate both STAT1 and STAT2. As a result, an IFN-stimulated gene factor 3 (ISGF3) complex forms ' this contains STAT1, STAT2 and a third transcription factor called IRF9 ' and moves into the cell nucleus. Inside the nucleus, the ISGF3 complex binds to specific nucleotide sequences called IFN-stimulated response elements (ISREs) in the promoters of certain genes, known as IFN stimulated genes ISGs. Binding if ISGF3 and other trasncriptional complexes activated by IFN signaling to these specific regulatory elements induces transcription of those genes.[8] Interferome is an curated online database of ISGs (www.interferome.org); Additionally, STAT homodimers or heterodimers form from different combinations of STAT-1, -3, -4, -5, or -6 during IFN signaling; these dimers initiate gene transcription by binding to IFN-activated site (GAS) elements in gene promoters.[8] Type I IFNs can induce expression of genes with either ISRE or GAS elements, but gene induction by type II IFN can occur only in the presence of a GAS element.[8]
In addition to the JAK-STAT pathway, IFNs can activate several other signaling cascades. Both type I and type II IFNs activate a member of the CRK family of adaptor proteins called CRKL, a nuclear adaptor for STAT5 that also regulates signaling through the C3G/Rap1 pathway.[8] Type I IFNs further activate p38 mitogen-activated protein kinase (MAP kinase) to induce gene transcription.[8] Antiviral and antiproliferative effects specific to type I IFNs result from p38 MAP kinase signaling. The phosphatidylinositol 3-kinase (PI3K) signaling pathway is also regulated by both type I and type II IFNs. PI3K activates P70-S6 Kinase 1, an enzyme that increases protein synthesis and cell proliferation; phosphorylates of ribosomal protein s6, which is involved in protein synthesis; and phosphorylates a translational repressor protein called eukaryotic translation-initiation factor 4E-binding protein 1 (EIF4EBP1) in order to deactivate it.[8]
[edit] Virus resistance to interferons
Many viruses have evolved mechanisms to resist interferon activity.[9] They circumvent the IFN response by blocking downstream signaling events that occur after the cytokine binds to its receptor, by preventing further IFN production, and by inhibiting the functions of proteins that are induced by IFN.[10] Viruses that inhibit IFN signaling include Japanese Encephalitis Virus (JEV), dengue type 2 virus (DEN-2) and viruses of the herpesvirus family, such as human cytomegalovirus (HCMV) and Kaposi's sarcoma-associated herpesvirus (KSHV or HHV8).[10][11] Viral proteins proven to affect IFN signaling include EBV nuclear antigen 1 (EBNA1) and EBV nuclear antigen 2 (EBNA-2) from Epstein-Barr virus, the large T antigen of Polyomavirus, the E7 protein of Human papillomavirus (HPV), and the B18R protein of vaccinia virus.[11][12] Reducing IFN-î� activity may prevent signaling via STAT1, STAT2, or IRF9 (as with JEV infection) or through the JAK-STAT pathway (as with DEN-2 infection).[10] Several poxviruses encode soluble IFN receptor homologs'like the B18R protein of the vaccinia virus'that bind to and prevent IFN interacting with its cellular receptor, impeding communication between this cytokine and its target cells.[12] Some viruses can encode proteins that bind to double-stranded RNA (dsRNA) to prevent the activity of RNA-dependent protein kinases; this is the mechanism reovirus adopts using its sigma 3 (σ3) protein, and vaccinia virus employs using the gene product of its E3L gene, p25.[13][14][15] The ability of interferon to induce protein production from interferon stimulated genes (ISGs) can also be affected. Production of protein kinase R, for example, can be disrupted in cells infected with JEV or flaviviruses.[10] Some viruses escape the anti-viral activities of interferons by gene (and thus protein) mutation. The H5N1 influenza virus, also known as bird flu, has resistance to interferon and other anti-viral cytokines that is attributed to a single amino acid change in its Non-Structural Protein 1 (NS1), although the precise mechanism of how this confers immunity is unclear.[16]
[edit] Interferon therapy
[edit] Diseases
The immune effects of interferons have been exploited to treat several diseases. Agents that activate the immune system, such as small imidazoquinoline molecules that activate TLR7, can induce IFN-î�. Imidazoquinoline is the main ingredient of Aldara (Imiquimod) cream, a treatment approved in the United States by the Food and Drug Administration (FDA) for actinic keratosis, superficial basal cell carcinoma, papilloma and external genital warts.[17] Synthetic IFNs are also made, and administered as antiviral, antiseptic and anticarcinogenic drugs, and to treat some autoimmune diseases.
Interferon beta-1a and interferon beta-1b are used to treat and control multiple sclerosis, an autoimmune disorder. This treatment is effective for slowing disease progression and activity in relapsing-remitting multiple sclerosis and reducing attacks in secondary progressive multiple sclerosis.[18]
Interferon therapy is used (in combination with chemotherapy and radiation) as a treatment for many cancers.[17] This treatment is most effective for treating hematological malignancy; leukemia and lymphomas including hairy cell leukemia, chronic myeloid leukemia, nodular lymphoma, cutaneous T-cell lymphoma.[17] Patients with recurrent melanomas receive recombinant IFN-î�2b.[19]
Both hepatitis B and hepatitis C are treated with IFN-î�, often in combination with other antiviral drugs.[20][21] Some of those treated with interferon have a sustained virological response and can eliminate hepatitis virus. The most harmful strain - hepatitis C genotype I virus - can only be treated around 50% of time by the standard of care treatment of interferon-î�/ribavirin.[22] Given the treatment, biopsies show reductions in liver damage and cirrhosis. Some evidence shows giving interferon immediately following infection can prevent chronic hepatitis C, although diagnosis early in infection is difficult since physical symptoms are sparse in early hepatitis C infection. Control of chronic hepatitis C by IFN is associated with reduced hepatocellular carcinoma.[23]
Administered intranasally in very low doses, interferon is extensively used in Eastern Europe and Russia as a method to prevent and treat viral respiratory diseases such as cold and flu. However, mechanisms of such action of interferon are not well understood; it is thought that doses must be larger by several orders of magnitude to have any effect on the virus. Although most Western scientists are skeptical of any claims of good efficacy,[24] recent findings suggest that interferon applied to mucosa may act as an adjuvant against influenza virus, boosting the specific immune system response against the virus. [23] A flu vaccine that uses interferon as adjuvant is currently under clinical trials in the US.[25]
When used in the systemic therapy, IFNs are mostly administered by an intramuscular injection. The injection of IFNs in the muscle, in the vein, or under skin is generally well tolerated. The most frequent adverse effects are flu-like symptoms: increased body temperature, feeling ill, fatigue, headache, muscle pain, convulsion, dizziness, hair thinning, and depression. Erythema, pain and hardness on the spot of injection are also frequently observed. IFN therapy causes immunosuppression, in particular through neutropenia and can result in some infections manifesting in unusual ways.[26]
[edit] Drug formulations
| Generic name | Trade name |
|---|---|
| Interferon alpha 2a | Roferon A |
| Interferon alpha 2b | Intron A/Reliferon |
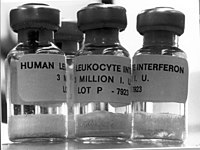
| Human leukocyte Interferon-alpha (HuIFN-alpha-Le) | Multiferon |
| Interferon beta 1a, liquid form | Rebif |
| Interferon beta 1a, lyophilized | Avonex |
| Interferon beta 1a, biogeneric (Iran) | Cinnovex |
| Interferon beta 1b | Betaseron / Betaferon |
| PEGylated interferon alpha 2a | Pegasys |
| PEGylated interferon alpha 2a (Egypt) | Reiferon Retard |
| PEGylated interferon alpha 2b | PegIntron |
| PEGylated interferon alpha 2b plus ribavirin (Canada) | Pegetron |
Several different types of interferon are now approved for use in humans. By March 10, 2009, MultiferonTM ' known generically as human leukocyte interferon-alpha (HuIFN-alpha-Le) ' was being used in 14 European countries. This drug was approved for treatment of patients with high risk (stage IIb-III) cutaneous melanoma, after 2 treatment cycles with dacarbazine, following a clinical trial performed in Germany.[27][28][29]
In January 2001, the Food and Drug Administration (FDA) approved the use of PEGylated interferon-alpha in the USA; in this formulation, polyethylene glycol is added to make the interferon last longer in the body. Initially used for production of PEGylated interferon-alpha-2b (Pegintron), approval for PEGylated interferon-alpha-2a (Pegasys) followed in October 2002. These PEGylated drugs are injected once weekly, rather than administering three times per week, as is necessary for conventional interferon-alpha. When used with the antiviral drug ribavirin, PEGylated interferon is effective in treatment of hepatitis C; at least 75% people with hepatitis C genotypes 2 or 3 benefit from interferon treatment, although this is effective in less than 50% of people infected with genotype 1 (the more common form of hepatitis C virus in both the U.S. and Western Europe).[30][31][32]
[edit] History
During research to produce a more efficient vaccine for smallpox, Yasu-ichi Nagano and Yasuhiko Kojima ' two Japanese virologists working at the Institute for Infectious Diseases at the University of Tokyo ' noticed inhibition of viral growth in an area of rabbit-skin or testis previously inoculated with UV-inactivated virus. They hypothesised that some "viral inhibitory factor" was present in the tissues infected with virus and attempted to isolate and characterize this factor from tissue homogenates. In 1954, these findings were published in a French journal now known as 'Journal de la Société de Biologie'.[33] After Nagano and Kojima separated the viral inhibitory factor from the viral particles using Ultracentrifugation, they confirmed its antiviral activity lasted 1'4 days and did not result from antibody production; their findings were published in 1958.[34][35][36] Nagano's work was never fully appreciated in the scientific community; possibly because it was printed in French, but also because his in vivo system was perhaps too complex to provide clear results in the characterisation and purification of interferon.[37]
Meanwhile, the British virologist Alick Isaacs and the Swiss researcher Jean Lindenmann, at the National Institute for Medical Research in London, noticed an interference effect caused by heat-inactivated influenza virus on the growth of live influenza virus in chicken egg chorioallantoic membrane. They published their results, attaining wide recognition, in 1957;[38] in this paper they coined the term 'interferon', and today that specific interfering agent is known as a 'Type I interferon'.[39] The majority of the credit for discovery of the interferon goes to Isaacs and Lindenmann, with whom there is no record of Nagano ever having made personal contact.[37] The purification of interferons did not occur until 1978. A series of publications from the laboratories of Sidney Pestka and Alan Waldman between 1978 and 1981, describe the purification of the type I interferons IFN-î� and IFN-î�.[40] By the early 1980s, the genes for these interferons were cloned allowing ' for the first time ' definitive proof that interferons really were responsible for interfering with viral replication.[41][42] Gene cloning also confirmed that IFN-î� was encoded by, not one gene, but a family of related genes.[43] The type II IFN (IFN-î�) gene was also isolated around this time.[44]
Interferon was scarce and expensive until 1980 when the interferon gene was inserted into bacteria using recombinant DNA technology, allowing mass cultivation and purification from bacterial cultures[45] or derived from yeast (e.g. Reiferon Retard is the first yeast derived interferon-alpha 2a).
[edit] See also
[edit] References
- ^ Liu YJ (2005). "IPC: professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors". Annu Rev Immunol 23: 275'306. doi:10.1146/annurev.immunol.23.021704.115633. PMID 15771572.
- ^ Vilcek, Novel interferons. Nature Immunology, 2003, Volume 4, pages 8-9
- ^ Fensterl, V; Sen GC (2009). "Interferons and viral infections". Biofactors 35 (1): 14'20. doi:10.1002/biof.6. PMID 19319841.
- ^ de Veer, MJ; Holko M, Frevel M, Walker E, Der S, Paranjape JM, Silverman RH, Williams BR (2001). "Functional classification of interferon-stimulated genes identified using microarrays". Journal of leukocyte biology 69 (6): 912'20. PMID 11404376.
- ^ a b Takaoka A, Hayakawa S, Yanai H, et al. (2003). "Integration of interferon-alpha/beta signalling to p53 responses in tumour suppression and antiviral defence". Nature 424 (6948): 516'23. doi:10.1038/nature01850. PMID 12872134. http://www.nature.com/nature/journal/v424/n6948/pdf/nature01850.pdf.
- ^ Moiseeva O, Mallette FA, Mukhopadhyay UK, Moores A, Ferbeyre G (2006). "DNA damage signaling and p53-dependent senescence after prolonged beta-interferon stimulation". Mol. Biol. Cell 17 (4): 1583'92. doi:10.1091/mbc.E05-09-0858. PMID 16436515.
- ^ Haller, O; Kochs G, Weber F. (October-Dec 2007). "Interferon, Mx, and viral countermeasures". Cytokine Growth Factor Rev. 18 (5-6): 425'33. doi:10.1016/j.cytogfr.2007.06.001. PMID 17683972.
- ^ a b c d e f g h Platanias, L. C. (May 2005). "Mechanisms of type-I- and type-II-interferon-mediated signalling". Nature reviews. Immunology 5 (5): 375'386. doi:10.1038/nri1604. ISSN 1474-1733. PMID 15864272.
- ^ Navratil V, de Chassey B, et al. (2010-11-05). "Systems-level comparison of protein-protein interactions between viruses and the human type I interferon system network.". Journal of Proteome Research 9 (7): 3527'36. doi:10.1021/pr100326j. PMID 20459142.
- ^ a b c d Lin RJ, Liao CL, Lin E, Lin YL (2004 aaa). "Blocking of the alpha interferon-induced Jak-Stat signaling pathway by Japanese encephalitis virus infection". J. Virol. 78 (17): 9285'94. doi:10.1128/JVI.78.17.9285-9294.2004. PMID 15308723.
- ^ a b Sen GC (2001). "Viruses and interferons". Annu. Rev. Microbiol. 55: 255'81. doi:10.1146/annurev.micro.55.1.255. PMID 11544356.
- ^ a b Alcamí A, Symons JA, Smith GL (December 2000). "The vaccinia virus soluble alpha/beta interferon (IFN) receptor binds to the cell surface and protects cells from the antiviral effects of IFN". J. Virol. 74 (23): 11230'9. doi:10.1128/JVI.74.23.11230-11239.2000. PMID 11070021. PMC 113220. http://jvi.asm.org/cgi/pmidlookup?view=long&pmid=11070021.
- ^ Minks MA, West DK, Benvin S, Baglioni C (October 1979). "Structural requirements of double-stranded RNA for the activation of 2',5'-oligo(A) polymerase and protein kinase of interferon-treated HeLa cells". J. Biol. Chem. 254 (20): 10180'3. PMID 489592. http://www.jbc.org/cgi/pmidlookup?view=long&pmid=489592.
- ^ Miller JE, Samuel CE (September 1992). "Proteolytic cleavage of the reovirus sigma 3 protein results in enhanced double-stranded RNA-binding activity: identification of a repeated basic amino acid motif within the C-terminal binding region". J. Virol. 66 (9): 5347'56. PMID 1501278. PMC 289090. http://jvi.asm.org/cgi/pmidlookup?view=long&pmid=1501278.
- ^ Chang HW, Watson JC, Jacobs BL (June 1992). "The E3L gene of vaccinia virus encodes an inhibitor of the interferon-induced, double-stranded RNA-dependent protein kinase". Proc. Natl. Acad. Sci. U.S.A. 89 (11): 4825'9. doi:10.1073/pnas.89.11.4825. PMID 1350676. PMC 49180. http://www.pnas.org/cgi/pmidlookup?view=long&pmid=1350676.
- ^ Sang Heui Seo, Erich Hoffmann, Robert G. Webster (August 2002). "Lethal H5N1 influenza viruses escape host anti-viral cytokine responses". Nature Medicine 8 (9): 950'954. doi:10.1038/nm757. PMID 12195436. http://www.nature.com/nm/journal/v8/n9/full/nm757.html.
- ^ a b c Goldstein, D; Laszlo, J (Sep 1988). "The role of interferon in cancer therapy: a current perspective" (Free full text). CA: a cancer journal for clinicians 38 (5): 258'77. doi:10.3322/canjclin.38.5.258. ISSN 0007-9235. PMID 2458171. http://caonline.amcancersoc.org/cgi/pmidlookup?view=long&pmid=2458171.
- ^ Paolicelli, D; Direnzo, V; Trojano, M (14 September 2009). "Review of interferon beta-1b in the treatment of early and relapsing multiple sclerosis" (Free full text). Biologics : targets & therapy 3: 369'76. ISSN 1177-5475. PMID 19707422. PMC 2726074. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=19707422.
- ^ Hauschild, A.; Gogas, H.; Tarhini, A.; Middleton, M.; Testori, A.; Dréno, B.; Kirkwood, J. (Mar 2008). "Practical guidelines for the management of interferon-alpha-2b side effects in patients receiving adjuvant treatment for melanoma: expert opinion". Cancer 112 (5): 982'994. doi:10.1002/cncr.23251. ISSN 0008-543X. PMID 18236459.
- ^ Cooksley, WG (Mar 2004). "The role of interferon therapy in hepatitis B". MedGenMed : Medscape general medicine 6 (1): 16. PMID 15208528.
- ^ Shepherd, J; Waugh, N; Hewitson, P (2000). "Combination therapy (interferon alfa and ribavirin) in the treatment of chronic hepatitis C: a rapid and systematic review" (Free full text). Health technology assessment (Winchester, England) 4 (33): 1'67. ISSN 1366-5278. PMID 11134916. http://www.hta.ac.uk/execsumm/summ433.htm.
- ^ Ge D, Fellay J, Thompson AJ, et al. (2009). "Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance". Nature 461 (7262): 399'401. doi:10.1038/nature08309. PMID 19684573.
- ^ a b Ishikawa, T (Oct 2008). "Secondary prevention of recurrence by interferon therapy after ablation therapy for hepatocellular carcinoma in chronic hepatitis C patients" (Free full text). World journal of gastroenterology : WJG 14 (40): 6140'4. doi:10.3748/wjg.14.6140. ISSN 1007-9327. PMID 18985803. PMC 2761574. http://www.wjgnet.com/1007-9327/14/6140.asp.
- ^ Joseph M. Cummins, DVM, PhD and Chad G. Thompson, BA. Low Dose Interferon, Immune Modulation and Emergency Influenza Prophylaxis. Amarillo Biosciences. http://www.pathobiologics.org/ivphc/ref/iav121604.doc. Retrieved 2010-07-14.
- ^ "Interferon as a Mucosal Adjuvant for Influenza Vaccine Given Intranasally - Full Text View". ClinicalTrials.gov. http://clinicaltrials.gov/ct2/show/NCT00436046. Retrieved 2010-07-14.
- ^ Bhatti Z, Berenson CS (2007). "Adult systemic cat scratch disease associated with therapy for hepatitis C". BMC Infect Dis 7: 8. doi:10.1186/1471-2334-7-8. PMID 17319959.
- ^ stagehttps://en.wikipedia.orghttps://en.wikipedia.org/wiki/Melanoma#Staging
- ^ Läkemedelsverkerhttp 3 milj IE solu f inj pre-filled syringe ENG
- ^ Stadler, R., et al. "Long-term survival benefit after adjuvant treatment of cutaneous melanoma with dacarbazine and low dose natural interferon alpha: A controlled, randomised multicentre trial". Acta Oncologica, Volume 45, Issue 4 June 2006, pages 389'399.
- ^ Jamall IS, Yusuf S, Azhar M, Jamall S (November 2008). "Is pegylated interferon superior to interferon, with ribavarin, in chronic hepatitis C genotypes 2/3?". World J. Gastroenterol. 14 (43): 6627'31. doi:10.3748/wjg.14.6627. PMID 19034963.
- ^ "NIH Consensus Statement on Management of Hepatitis C: 2002". NIH Consens State Sci Statements 19 (3): 1'46. 2002. PMID 14768714.
- ^ Sharieff KA, Duncan D, Younossi Z (February 2002). "Advances in treatment of chronic hepatitis C: 'pegylated' interferons". Cleve Clin J Med 69 (2): 155'9. doi:10.3949/ccjm.69.2.155. PMID 11990646.
- ^ Nagano Y, Kojima Y (October 1954). "Pouvoir immunisant du virus vaccinal inactivé par des rayons ultraviolets" (in French). C. R. Seances Soc. Biol. Fil. 148 (19-20): 1700'2. PMID 14364998.
- ^ Ozato K, Uno K, Iwakura Y (May 2007). "Another road to interferon: Yasuichi Nagano's journey". J. Interferon Cytokine Res. 27 (5): 349'52. doi:10.1089/jir.2007.9988. PMID 17523866.
- ^ Nagano Y, Kojima Y (1958). "Inhibition de l'infection vaccinale par un facteur liquide dans le tissu infecté par le virus homologue" (in French). C. R. Seances Soc. Biol. Fil. 152 (11): 1627'9. PMID 13639454.
- ^ Watanabe Y (December 2004). "Fifty years of interference". Nat. Immunol. 5 (12): 1193. doi:10.1038/ni1204-1193. PMID 15549114.
- ^ a b International Society For Interferon And Cytokine Research, October 2005 Volume 12, No. 3.
- ^ Isaacs A, Lindenmann J (September 1957). "Virus interference. I. The interferon". Proc. R. Soc. Lond., B, Biol. Sci. 147 (927): 258'67. doi:10.1098/rspb.1957.0048. PMID 13465720.
- ^ Mergiran, TC. Worldbook Science Year, 1980
- ^ Pestka S (July 2007). "The interferons: 50 years after their discovery, there is much more to learn". J. Biol. Chem. 282 (28): 20047'51. doi:10.1074/jbc.R700004200. PMID 17502369.
- ^ Weissenbach J, Chernajovsky Y, Zeevi M, et al. (December 1980). "Two interferon mRNAs in human fibroblasts: in vitro translation and Escherichia coli cloning studies". Proc. Natl. Acad. Sci. U.S.A. 77 (12): 7152'6. doi:10.1073/pnas.77.12.7152. PMID 6164058.
- ^ Taniguchi T, Fujii-Kuriyama Y, Muramatsu M (July 1980). "Molecular cloning of human interferon cDNA". Proc. Natl. Acad. Sci. U.S.A. 77 (7): 4003'6. doi:10.1073/pnas.77.7.4003. PMID 6159625.
- ^ Nagata S, Mantei N, Weissmann C (October 1980). "The structure of one of the eight or more distinct chromosomal genes for human interferon-alpha". Nature 287 (5781): 401'8. doi:10.1038/287401a0. PMID 6159536.
- ^ Gray PW, Goeddel DV (August 1982). "Structure of the human immune interferon gene". Nature 298 (5877): 859'63. doi:10.1038/298859a0. PMID 6180322.
- ^ Nagata S, Taira H, Hall A, et al. (March 1980). "Synthesis in E. coli of a polypeptide with human leukocyte interferon activity". Nature 284 (5754): 316'20. doi:10.1038/284316a0. PMID 6987533.
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
SOURCES.COM is an online portal and directory for journalists, news media, researchers and anyone seeking experts, spokespersons, and reliable information resources. Use SOURCES.COM to find experts, media contacts, news releases, background information, scientists, officials, speakers, newsmakers, spokespeople, talk show guests, story ideas, research studies, databases, universities, associations and NGOs, businesses, government spokespeople. Indexing and search applications by Ulli Diemer and Chris DeFreitas.
For information about being included in SOURCES as a expert or spokesperson see the FAQ . For partnerships, content and applications, and domain name opportunities contact us.